
A bone infection in the mouth, also known as osteomyelitis, is a serious condition that requires prompt medical attention. It's a bacterial infection that affects the bone and surrounding tissue.
Symptoms of bone infection in the mouth include severe pain, swelling, and redness in the affected area. A foul odor from the mouth is also a common symptom.
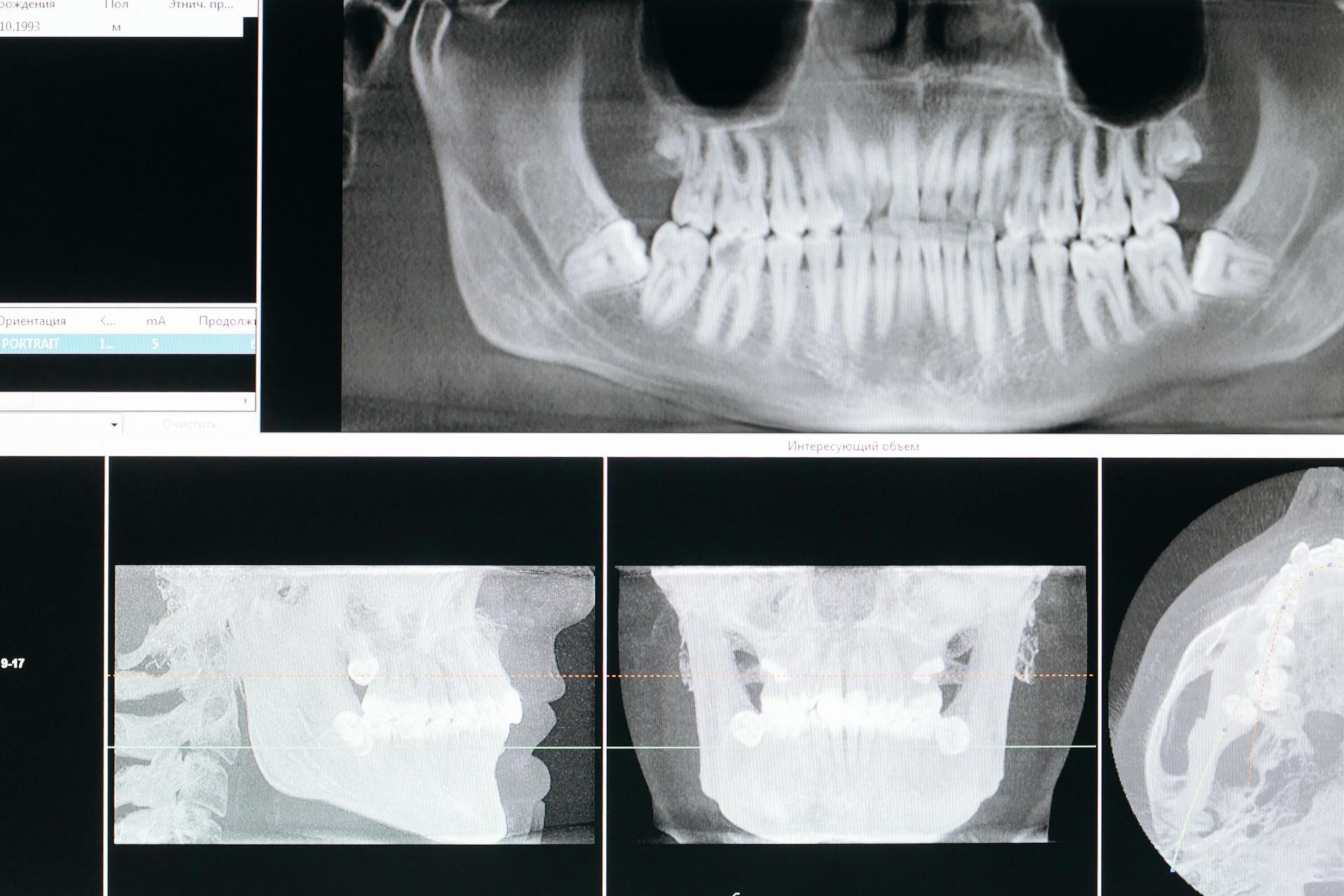
Diagnosing bone infection in the mouth typically involves a combination of physical examination, medical history, and imaging tests such as X-rays or CT scans. These tests can help identify the presence and extent of the infection.
Treatment for bone infection in the mouth usually involves antibiotics to fight the infection, and in some cases, surgery may be necessary to remove infected tissue.
What Is Bone Infection in Mouth?
Bone infection in the mouth is a serious condition that occurs when bacteria infect the bone tissue.
The infection can be caused by a variety of factors, including gum disease, dental cavities, and trauma to the mouth.
Bacteria from gum disease can penetrate deep into the bone, causing an infection known as osteomyelitis.
In some cases, the infection can be caused by a dental procedure gone wrong, such as a root canal or extraction.
Symptoms of bone infection in the mouth can include pain, swelling, and a foul odor.
The pain can be severe and may be constant or come and go.
In some cases, the infection can cause a fever, which can be a sign of a more serious infection.
If left untreated, bone infection in the mouth can lead to serious complications, such as the spread of infection to other parts of the body.
Causes and Risk Factors
Dental infections can progress and infect the jaw bone if left untreated.
Tooth decay, abscesses, or untreated gum disease are common culprits that can lead to jaw bone infections.
Tooth extraction or implant placement procedures can risk introducing bacteria into the bone, increasing the risk of infection.
Accidents or injuries that result in fractures or breaks in the jaw bone can provide an entry point for bacteria.
Individuals with weakened immune systems, such as those with diabetes or undergoing chemotherapy, are more susceptible to infections.
Some people may be more prone to jaw bone infections due to the following factors:
- Tobacco and nicotine use can obstruct bone healing.
- Antibiotics and corticosteroids can interfere with the healing process.
- Heredity or acquired clotting disorders can increase the risk of infection.
- Excessive use of NSAIDs can slow down bone healing.
- Presence of heavy metals like copper, mercury, silver, and iron can contribute to infection.
- Trauma from dental surgery can increase the risk of infection.
- Radiation and chemotherapy can weaken the immune system.
Symptoms and Complications
A jawbone infection can be quite painful and uncomfortable. Persistent and severe pain in the jaw area is a common symptom.
Swelling and redness around the infected site can be a sign that the infection is serious. Facial swelling is another possible indication of a jawbone infection.
If you're experiencing fever and general malaise, it could be a sign that your body is fighting an infection. Difficulty opening the mouth or chewing is another symptom to watch out for.
Here are some possible complications of a jawbone infection:
- Spread of infection to surrounding tissues, including the face and neck
- Formation of abscesses or pockets of pus
- Damage to adjacent teeth and gums
- Necrosis (death) of bone tissue
- Septicemia (blood infection) and systemic complications
Symptoms
Symptoms of a jawbone infection can be quite painful and uncomfortable. Pain in the mouth or jaw is one of the first signs, often accompanied by jaw stiffness.

You may also notice facial swelling, which can be a red and tender area. Redness and tenderness are common symptoms, making it difficult to ignore the issue.
Here are some possible symptoms to look out for:
- Persistent and severe pain in the jaw area
- Swelling and redness around the infected site
- Fever and general malaise
- Difficulty opening the mouth or chewing
- Drainage of pus or discharge from the gums
If left untreated, a jawbone infection can lead to serious complications, such as the spread of infection to surrounding tissues, including the face and neck.
Necrosis (Osteomyelitis)
Necrosis (Osteomyelitis) can be a serious complication of chronic periapical infection.
Osteomyelitis is a common sequel of chronic periapical infection.
This type of infection can also be caused by pathologies that obstruct blood supply, leading to ischemia and bone death.
Bone death and necrosis can occur due to osteomyelitis, which can be acute or chronic in nature.
The main difference between acute and chronic osteomyelitis is the time limit of a month after the onset of disease.
The acute form of osteomyelitis is more common and is the focus of urgent care scenarios.
Treatment Options
Treatment options for a bone infection in the mouth depend on the severity and extent of the infection. In mild cases, antibiotics may be prescribed to eliminate the bacteria causing the infection.
Antibiotics can be effective in treating jaw infections caused by bacterial infections, and amoxicillin is a highly effective medication for this purpose. It's essential to complete the course of antibiotics as prescribed by your healthcare provider.
Surgical debridement, a procedure in which infected or dead tissue is removed from the wound, may also be necessary to promote healing. This can help reduce the number of bacteria present and promote healing.
In more severe cases, surgery may be required to drain and clean the infected area, followed by antibiotics. A bone graft may also be necessary in some cases to repair and rebuild the damaged bone.
Here are some common treatment options for bone infection in the mouth:
- Antibiotics: prescribed in the form of pills or intravenous (IV) infusion
- Surgical debridement: to remove infected or dead tissue
- Surgery: to drain and clean the infected area and remove infected bone
- Bone graft: to repair and rebuild damaged bone
It's essential to follow the treatment plan prescribed by your healthcare provider to effectively treat the bone infection and prevent it from spreading or recurring.
Core Importance of Prompt Dental Care
Seeking prompt dental care is crucial when dealing with a jawbone infection. Ignoring or delaying treatment can lead to the infection worsening and potential complications.
If you experience any signs or symptoms of a jawbone infection, it's essential to visit your dentist or oral surgeon as soon as possible. They will evaluate your condition, diagnose properly, and recommend the most appropriate treatment plan.
In severe cases, dental procedures may be necessary to remove the source of infection and promote healing. These procedures can include root canal treatment, tooth extraction, or bone grafting.
Here are some common dental procedures that may be necessary to address a jawbone infection:
- Root Canal Treatment: removes the infected pulp and disinfects the root canal system
- Tooth Extraction: eliminates the source of infection if the tooth is severely damaged or cannot be saved
- Bone Grafting: restores the jaw bone's structure and promotes regeneration if the infection has caused significant bone loss
Diagnosis and Testing
To diagnose a bone infection in the mouth, your doctor will conduct a physical examination to check for tenderness, swelling, or warmth around the affected bone.
They will also perform blood tests to see if your body is fighting an infection. Elevated levels of white blood cells and other factors in your blood can indicate an infection.
Imaging tests, such as X-rays, MRI, and CT scans, can reveal bone damage and help confirm the diagnosis. MRI produces highly detailed images of bones and soft tissues, while CT scans are used when an MRI is not feasible.
Osteomyelitis can be misdiagnosed due to its symptoms resembling other jaw, skull, or face conditions. To rule out other conditions, your doctor may consider differential diagnoses such as osteoradionecrosis and bisphosphonate-related osteonecrosis of the jaw.
The following tests may be used to diagnose a bone infection in the mouth:
- Blood tests
- X-rays
- MRI
- CT scans
Treatment and Extraction
Treatment and extraction are often necessary to remove the source of infection and promote healing. This can involve a range of procedures, including root canal treatment, tooth extraction, and bone grafting.
Antibiotics may be prescribed to kill or inhibit the growth of bacteria, and surgical debridement may be performed to remove infected or dead tissue. This can help reduce the number of bacteria present and promote healing.

In some cases, further surgery may be necessary to remove the infected bone, which is called an open drainage procedure. This involves making an incision in the skin to allow the infection to drain out.
To determine the best course of treatment, it's essential to follow the treatment plan prescribed by your healthcare provider. This may involve regular follow-ups with your dentist to ensure the infection is being effectively treated and to prevent it from spreading or recurring.
Treatment options may include:
- Antibiotics
- Surgical debridement
- Root canal treatment
- Tooth extraction
- Bone grafting
Extraction Treatment
Tooth extraction is a common treatment for bone infections after a tooth extraction. This procedure involves removing the infected tooth to eliminate the source of infection.
In some cases, antibiotics may be sufficient to treat the infection, but in more severe cases, tooth extraction is necessary. Regular follow-ups with your dentist are crucial to monitor the healing process.
The healing process of jawbone infections might take a while, but with proper treatment, you can recover. Natural disinfectants can kill bacteria, viruses, fungi, and other residual microorganisms, promoting healing.
Here are some common procedures that may be necessary after tooth extraction:
- Antibiotics: prescribed to kill or inhibit the growth of bacteria
- Surgical debridement: a procedure to remove infected or dead tissue from the wound
- Tooth extraction: removing the infected tooth to eliminate the source of infection
- Surgery: in some cases, further surgery may be necessary to remove the infected bone
Surgical Intervention
Surgical Intervention can be a necessary step in treating severe cases of infection. In rare instances, you may require surgical intervention to remove infected bone tissue and promote healing.
Debridement is a procedure where the oral surgeon removes the infected or dead bone to prevent the spread of infection. This helps to prevent the infection from getting worse.
Bone grafting may also be performed to replace the removed bone and facilitate regeneration. This can help to restore the health of the affected area and promote healing.
Extraction
If you're experiencing severe tooth damage or infection, tooth extraction may be necessary to eliminate the source of the problem. This is a common procedure that can be performed by a dentist or oral surgeon.
Tooth extraction is usually a last resort, but it's a viable option when other treatments aren't working. In fact, about 5 million people in the United States undergo tooth extraction every year.
If you're experiencing a jaw bone infection after tooth extraction, you may need to undergo additional procedures to promote healing. These can include antibiotics, surgical debridement, and in some cases, further surgery to remove the infected bone.
In some cases, dental procedures may be necessary to remove the source of infection and promote healing. These can include root canal treatment, tooth extraction, and bone grafting.
Here are some common symptoms that may indicate the need for tooth extraction:
• Pain or swelling at the extraction site that doesn't go away or gets worse over time
• Drainage of pus or blood from the extraction site
• Fever
• Swelling of the face or neck
• Difficulty opening the mouth
• Bad taste in the mouth
These symptoms can be a sign of a more serious underlying issue, so it's essential to seek medical attention if you're experiencing any of them.
Aftercare and Prevention
After a bone infection in the mouth is treated, it's essential to follow a proper aftercare routine to prevent further complications. This includes keeping the mouth clean by rinsing with salt water several times a day.
Regular dental check-ups are crucial to monitor the infection and prevent its recurrence. This can help identify any potential issues early on.
To prevent bone infection in the mouth, maintaining good oral hygiene is key. Brushing and flossing regularly can help prevent bacteria from accumulating and causing infection.
Complications and Outcomes
If left untreated, a jaw bone infection can lead to serious complications.
Spread of infection to surrounding tissues, including the face and neck, is a possible outcome. This can have severe consequences, including damage to the surrounding tissue and potentially life-threatening conditions.
Formation of abscesses or pockets of pus is another complication that can arise from a jaw bone infection. These abscesses can be painful and may require surgical drainage.
Damage to adjacent teeth and gums is a common complication of a jaw bone infection. This can lead to tooth loss and gum disease, making it essential to seek medical attention promptly.
Necrosis, or death, of bone tissue can occur if the infection is left untreated. This can result in permanent damage to the jaw bone and surrounding tissues.
Here are some potential complications of a jaw bone infection:
- Spread of infection to surrounding tissues
- Formation of abscesses or pockets of pus
- Damage to adjacent teeth and gums
- Necrosis (death) of bone tissue
- Septicemia (blood infection) and systemic complications
Frequently Asked Questions
How long does a jaw bone infection take to heal?
Typically, a jaw bone infection can take 3 to 5 days to clear up if treated promptly, but antibiotics are usually taken for 4 to 12 weeks to ensure complete recovery
Sources
- https://juliandental.com/blog/how-serious-is-a-jaw-bone-infection/
- https://neeshatkhandds.com/blog/how-serious-is-a-jaw-bone-infection/
- https://yourdoctors.online/jaw-bone-infection/
- https://jcda.ca/g13
- https://chengdds.com/dont-ignore-the-warning-signs-spotting-bone-infection-after-tooth-extraction-symptoms
Featured Images: pexels.com


